It’s no secret that well-being is subject to a kaleidoscope of variables, but biology, socioeconomics, environment, and lifestyle are just a few we know about. Adverse Childhood Experiences (ACEs) are lesser-known factors getting more press these days. Understanding their nature, prevalence, and profound influence on adult well-being is vitally important to health enhancement professionals. While ACEs can throw a serious wrench in the gears, they’re also preventable and treatable.
The body of knowledge around consequences — and how to help kids and adults heal — keeps growing, offering opportunities to promote awareness, prevention, and access to resources.
Evaluating ACE Impact
The presence of ACEs is assessed through questions about these experiences before the 18th birthday:
- Abuse (emotional, physical, sexual)
- Neglect (emotional, physical)
- Household challenges (like parental separation or divorce, mental illness, and substance abuse).
ACE scores are tabulated on a scale of 1-10; the higher the score, the more severe the potential effect on health and well-being. (See the graphic below, then view the complete ACE questionnaire.)
Below the Surface
A groundbreaking 1998 CDC-Kaiser Permanente study shed light on this important issue.1 These experiences are strikingly common, occurring across all socioeconomic and racial groups. In the original ACE study and CDC’s Behavioral Risk Factor Surveillance System, 2/3 of surveyed adults reported at least 1; more than 1 in 5 reported having at least 3 ACEs. Compared to none, for example, having 4 or more doubles the risk of heart disease, stroke, and cancer. In addition, ACEs are associated with increased risk for asthma, diabetes, depression, less education, unemployment, low income, disability, and more.
This doesn’t mean people with ACEs are doomed to a life of poor health and low potential; however, it does mean their level of risk is higher. Not surprisingly, regular exercise and not smoking, plus access to emotional support and other self-care factors, can make a significant difference; they’ve been linked with reports of excellent, very good, or good health among adults with ACEs.2
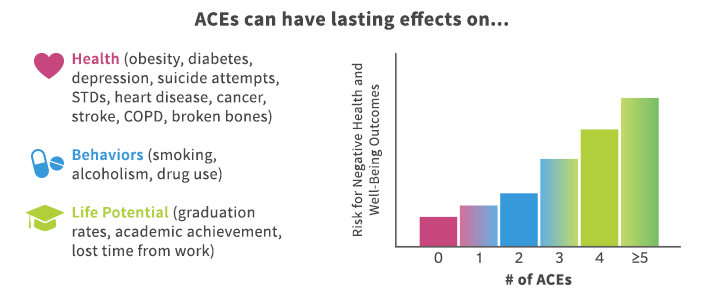
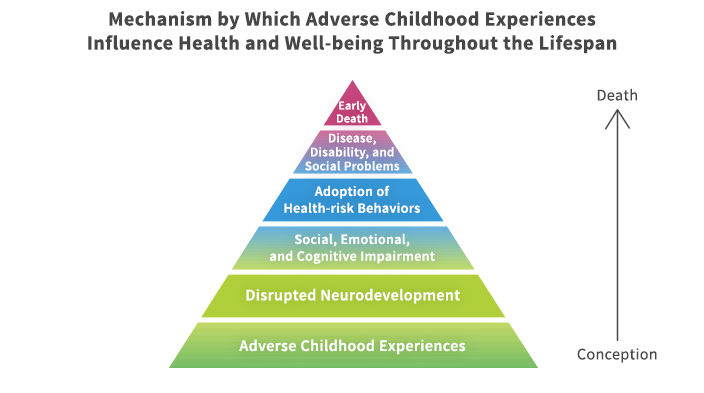
ACEs cause psychological trauma; they also change brain structure and function. The stress response is abnormal, chronically flooding vulnerable young brains and bodies with cortisol. As author and pediatrician Nadine Burke Harris, MD, MPH, explains, when adversity is strong, frequent, or prolonged, and when there is no caring adult to serve as a buffer, stress becomes toxic — consequently, this disrupts development in the brain and other organs. Kids with ACEs are more prone to develop health problems like asthma and obesity as well as significantly more likely to be diagnosed with learning and behavior problems.3 ACEs also wire childrens’ brains for negative beliefs… like low self-efficacy, shame, and self-blame, as shown in this CDC graphic.4
Evaluating and Treating the Root Cause
Pediatricians, internists, and other providers can use the ACE score to gain a more complete picture of patients’ well-being, then treat ACEs as the root cause of clinical conditions and symptoms as appropriate, referring them to clinical mental healthcare. Unfortunately, because many don’t use the ACE score due to a lack of training, their patients aren’t getting the treatment or services needed to reduce ACEs.
Another barrier is that many people don’t know about or understand the link between ACEs and adult well-being. When people realize that traumatic childhood experiences may negatively affect them today, they can seek help. With the right level of support, training, and resources, parents can protect children against ACEs and families can get the professional help they need to cope with trauma in healthy ways. Clinical mental healthcare enables kids and adults to process and heal from ACE trauma. And with support for lifestyle changes, they can adopt lasting self-care habits that reduce ACE impact on overall well-being. In time, they can feel and function better emotionally and physically — maybe for the first time in memory… and enjoy a better quality of life.
What to Do About ACEs
Besides cultivating a psychologically healthy work environment, what can well-being and HR leaders do? A few ideas:
- Teach your population about ACEs, how common they are, their effects, and what to do with the ACE score. Provide a link to the ACE questionnaire for a private self-assessment; include an easy way for people to share this information with their healthcare provider, like a printable document.
- Communicate the value of mental healthcare; address anxiety, depression, and other conditions in your wellness messaging just as you would asthma, heart disease, and arthritis. Convene a task force to strategize reducing the stigma of mental illness.
- Offer employer-sponsored services proven to help prevent ACEs: parenting training for moms and dads of infants through teens, coaching, discounts for high-quality childcare, mental illness and substance abuse treatment, violence prevention, and home visits to pregnant women and families with newborns and infants.5 Check with your public health agency to see if there’s a potential for partnership in delivering these services.
- Create self-care opportunities that promote personal and family well-being. Mindfulness-based stress reduction programs are beneficial;6 meditation resources and convenient quiet spaces promote practice. Onsite walking groups boost fitness and stress relief while cultivating personal connection. Benefits like flexible scheduling, concierge services, and dinners-to-go help prevent and reduce stress on the home front.
- Launch a challenge to build mental and emotional well-being through resilience, compassion, happiness, strong relationships, and more. The Greater Good in Action is an excellent resource.
- Use your purchasing power to push for provider training on ACEs, the questionnaire, and clinical practice implications.
- Advocate for co-located primary and behavioral health professionals to ease collaboration for more effective, convenient care.
- Team up with your EAP vendor to address the needs of employees and family members with ACEs using educational and community resources.
Family Protective Factors
Scientific evidence points to these factors for buffering children against abuse and neglect7:
- Supportive family environment and social networks
- Concrete support for basic needs
- Nurturing parenting skills
- Stable family relationships
- Household rules and child monitoring
- Parental employment
- Parental education
- Adequate housing
- Access to healthcare and social services
- Caring adults outside the family who can serve as role models or mentors.
Recommended Resources
- Shanta Dube: The Steps That Can Help Adults Heal From Childhood Trauma
- Nadine Burke Harris: How Does Trauma Affect A Child’s DNA?
- The Deepest Well: Healing the Long-Term Effects of Childhood Adversity, Houghton Mifflin Harcourt
- Adverse Childhood Experiences: Community Resources
References
1. Felitti VJ, Anda RF, Nordenberg D, et al. Relationship of Childhood Abuse and Household Dysfunction to Many of the Leading Causes of Death in Adults. American Journal of Preventive Medicine, May 1998, Volume 14, Issue 4, 245-25, ajpmonline.org/article/S0749-3797(98)00017-8/abstract
2. Dube, Shanta R. The Steps That Can Help Adults Heal From Childhood Trauma, The Conversation, 2017 theconversation.com/the-steps-that-can-help-adults-heal-from-childhood-trauma-77152
3. Burke Harris N. The Deepest Well: Healing the Long-Term Effects of Childhood Adversity, Houghton Mifflin Harcourt, 2018, 54-55
4. Martin B, Kendall-Tackett K. How to Overcome Adverse Childhood Experiences as an Adult, National Association of Adult Survivors of Child Abuse, accessed 7/24/18, naasca.org/2016-Articles/011116-OvercomingACE.htm
5. CDC, What Can Be Done About ACEs? cdc.gov/violenceprevention/acestudy/ACE_graphics.html
6. Hoge EA, Bui E, Marques L, et al. Randomized Controlled Trial of Mindfulness Meditation for Generalized Anxiety Disorder: Effects on Anxiety and Stress Reactivity. Journal of Clinical Psychiatry, 2013, Aug;74(8):786-92. doi: 10.4088/JCP.12m08083
7. cdc.gov/violenceprevention/childabuseandneglect/riskprotectivefactors.html
Beth Shepard
Well-being consultant, educator, writer |National Board Certified Health & Wellness Coach |Certified Lifestyle Medicine Coach|ACSM Certified Clinical Exercise Physiologist |25+ years in wellness |Jazz enthusiast.

